Cancer navigation is one of the few interventions that clearly improves patient experience, reduces delays, and closes care gaps. Yet across oncology practices, navigation programs routinely struggle financially. Navigators are hired, patients are helped, but the program quietly becomes a line item expense instead of a growth lever. When budgets are lean, navigators are often the first to be cut or the last position to be filled.
The problem is not navigation itself. It is how navigation is structured, measured, and operationalized.
The Hidden Structural Flaws in Most Navigation Programs
Most navigation programs grow organically. A practice hires a navigator to help patients who are struggling, overloaded staff start sending work their way, and responsibilities expand over time. What emerges is a well intentioned but structurally fragile model.
Common issues include:
- No defined scope of navigation activities versus clinical or administrative work
- No consistent intake or triage logic to determine who needs navigation and when
- Navigators operating reactively instead of within a defined workflow
- Success measured emotionally rather than operationally
- Dependence on philanthropy for financial survival
This creates three downstream problems. First, leadership cannot clearly articulate what value navigation delivers beyond “patients like it.” Second, the work becomes difficult to standardize, scale, or defend financially. Third, dependence of philanthropy creates uncertainty regarding regarding the future
Why Unstructured Navigation Is Invisible to Billing
Navigation struggles financially because it is rarely designed with billing in mind. Not because billing is unethical or secondary, but because most programs never map navigation work to billable services in a compliant way.
Unstructured navigation typically looks like:
- Phone calls without documented intent or outcomes
- Care coordination that is real but not coded
- Social support that addresses barriers but lacks standardized assessment
- Follow ups that are clinically useful but operationally vague
From a billing perspective, this work does not exist. Even when new navigation related CPT codes are available, practices struggle to use them because the underlying workflows were never built to support compliant documentation.
The result is a painful paradox. Practices are doing valuable work that costs real money, but the system has no way to see or reimburse it.
What Financially Sustainable Navigation Actually Looks Like
Sustainable navigation starts with treating it as a system, not a role.
Financially successful programs share several characteristics:
- Navigation activities are clearly defined and scoped
- Patients are risk stratified so navigation intensity matches need
- Every interaction has a documented purpose and outcome
- Workflows align with clinical pathways and payer requirements
- Navigation data is structured enough to support billing and reporting
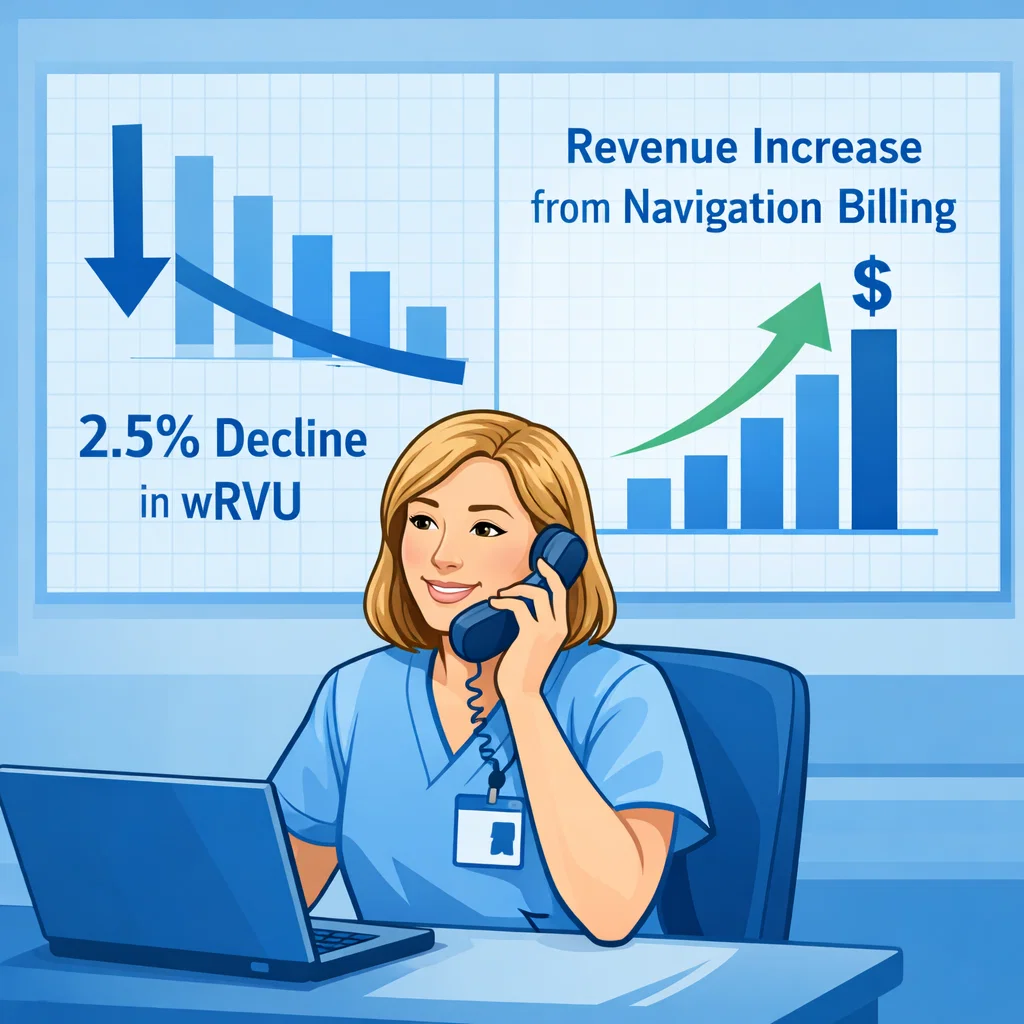
In this model, navigation stops being ad hoc support and becomes an operational function. Time to treatment, referral completion, barrier resolution, and out-migration reduction become measurable outputs. Documentation happens as a byproduct of care delivery, not an extra burden.
This is what allows navigation to move from a cost center to a revenue enabling service.
Fixing the Problem Without Burning Out Your Team
The biggest fear practices have is that “doing navigation right” means more clicks, more forms, and more staff fatigue. In reality, the opposite is true.
When navigation is standardized:
- Navigators spend less time improvising and more time executing
- Clinicians are shielded from non clinical coordination work
- Leadership gains visibility into throughput and leakage
- Billing becomes a natural extension of existing workflows
The long term fix is not simply hiring more navigators. It is designing navigation intentionally, with clear structure, measurable outcomes, and financial alignment from day one.
Navigation works. But only when it is built to be seen, measured, and sustained.
Book a demo of the XpediteMD platform to see how we can streamline patient navigation for your team, and make it financially sustainable.